Portal, AZ - Rodeo, NM
Serving The Communities Of Portal and Rodeo (www.portal-rodeo.com)
Serving The Communities Of Portal and Rodeo (www.portal-rodeo.com)

Ticks -Don’t Get Ticked Off
Ticks - Don’t Get Ticked Off
Tick exposure can occur year-round, but ticks are most active during warmer months (April-September). Know which ticks are most common in your area.
Before You Go Outdoors
• Know where to expect ticks. Ticks live in grassy, brushy, or wooded areas, or even on animals. Spending time outside walking your dog, camping, gardening, or hunting could bring you in close contact with ticks. Many people get ticks in their own yard or neighborhood.
• Treat clothing and gear with products containing 0.5% permethrin. Permethrin can be used to treat boots, clothing and camping gear and remain protective through several washings. Alternatively, you can buy permethrin-treated clothing and gear.
• Use Environmental Protection Agency (EPA)-registered insect repellentsexternal icon
containing DEET, picaridin, IR3535, Oil of Lemon Eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone.
Do not use products containing OLE or PMD on children under 3 years old.
• Avoid Contact with Ticks
◦ Avoid wooded and brushy areas with high grass and leaf litter.
◦ Walk in the center of trails.
After You Come Indoors
Check your clothing for ticks. Ticks may be carried into the house on clothing. Any ticks that are found should be removed. Tumble dry clothes in a dryer on high heat for 10 minutes to kill ticks on dry clothing after you come indoors. If the clothes are damp, additional time may be needed. If the clothes require washing first, hot water is recommended. Cold and medium temperature water will not kill ticks.
Examine gear and pets. Ticks can ride into the home on clothing and pets, then attach to a person later, so carefully examine pets, coats, and daypacks.
Shower soon after being outdoors. Showering within two hours of coming indoors has been shown to reduce your risk of getting Lyme disease and may be effective in reducing the risk of other tickborne diseases. Showering may help wash off unattached ticks and it is a good opportunity to do a tick check.
Check your body for ticks after being outdoors. Conduct a full body check upon return from potentially tick-infested areas, including your own backyard. Use a hand-held or full-length mirror to view all parts of your body. Check these parts of your body and your child’s body for ticks:
• Under the arms
• In and around the ears
• Inside belly button
• Back of the knees
• In and around the hair
• Between the legs
• Around the waist
Preventing Ticks On Your Pets
Dogs are very susceptible to tick bites and tickborne diseases. Vaccines are not available for most of the tickborne diseases that dogs can get, and they don’t keep the dogs from bringing ticks into your home. For these reasons, it’s important to use a tick preventive product on your dog.
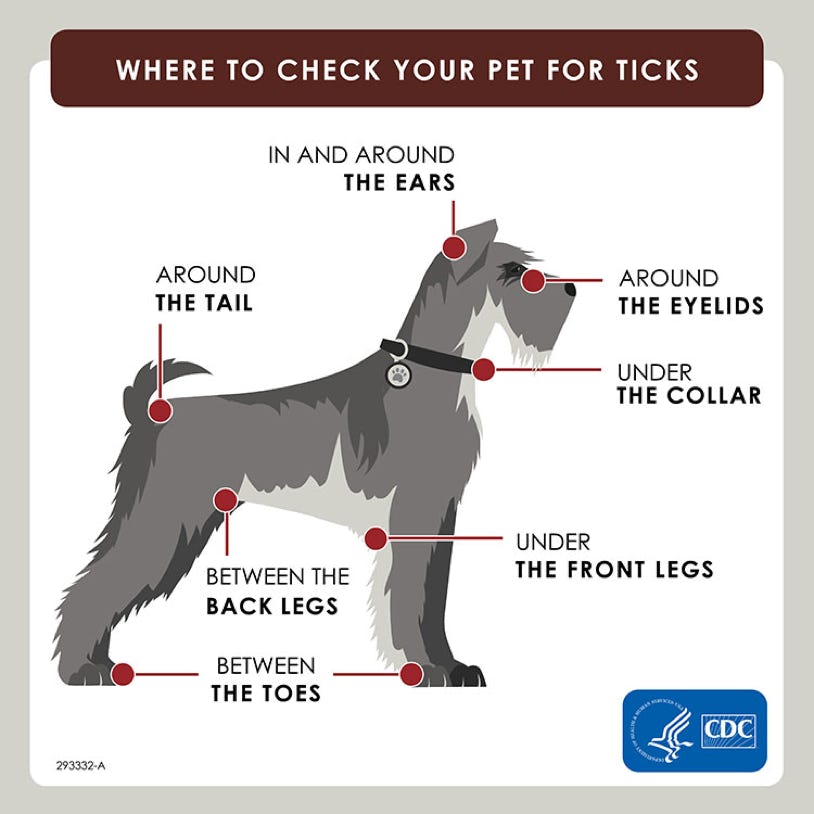
Tick bites on dogs may be hard to detect. Signs of tickborne disease may not appear for 7-21 days or longer after a tick bite, so watch your dog closely for changes in behavior or appetite if you suspect that your pet has been bitten by a tick.
Talk to your veterinarian about:
• The best tick prevention products for your dog
• Tickborne diseases in your area
To further reduce the chances that a tick bite will make your dog sick:
• Check your pets for ticks daily, especially after they spend time outdoors.
• If you find a tick on your pet, remove it right away.
• Reduce tick habitat in your yard.
Note: Cats are extremely sensitive to a variety of chemicals. Do not apply any tick prevention products to your cats without first asking your veterinarian!
Potential Adverse Events Associated with Isoxazoline Flea and Tick Products. For additional information, please talk to your veterinarian.
Preventing Ticks In The Yard
Apply Pesticides Outdoors to Control Ticks
Use of pesticides can reduce the number of ticks in treated areas of your yard. However, you should not rely on spraying to reduce your risk of infection.
When using pesticides, always follow label instructions. Before spraying, check with local health or agricultural officials about:
• The best time to apply pesticide in your area
• The best type of pesticide to use
• Here are some simple landscaping techniques that can help reduce blacklegged tick populations:
• Remove leaf litter.
• Clear tall grasses and brush around homes and at the edge of lawns.
• Place a 3-ft wide barrier of wood chips or gravel between lawns and wooded areas to restrict tick migration into recreational areas.
• Mow the lawn frequently.
• Stack wood neatly and in a dry area (discourages rodents).
• Keep playground equipment, decks, and patios away from yard edges and trees.
• Discourage unwelcome animals (such as deer, raccoons, and stray dogs) from entering your yard by constructing fences.
• Remove old furniture, mattresses, or trash from the yard that may give ticks a place to hide.
•
How To Remove A Tick
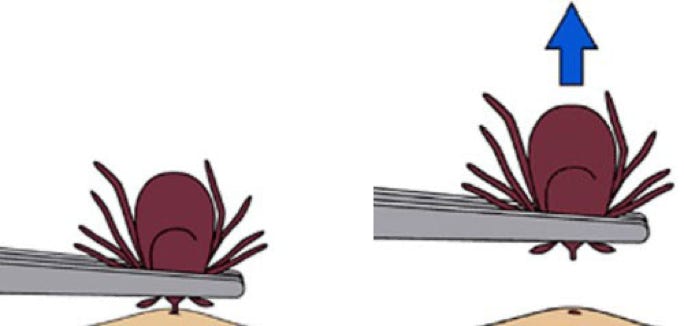
1. Use clean, fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible.
2. Pull upward with steady, even pressure. Don’t twist or jerk the tick; this can cause the mouth-parts to break off and remain in the skin. If this happens, remove the mouth-parts with tweezers. If you cannot remove the mouth easily with tweezers, leave it alone and let the skin heal.
3. After removing the tick, thoroughly clean the bite area and your hands with rubbing alcohol or soap and water.
4. Never crush a tick with your fingers. Dispose of a live tick by
◦ Putting it in alcohol,
◦ Placing it in a sealed bag/container,
◦ Wrapping it tightly in tape, or
◦ Flushing it down the toilet.
Follow-Up
If you develop a rash or fever within several weeks of removing a tick, see your doctor:
• Tell the doctor about your recent tick bite,
• When the bite occurred, and
• Where you most likely acquired the tick.
Avoid folklore remedies such as “painting” the tick with nail polish or petroleum jelly, or using heat to make the tick detach from the skin. Your goal is to remove the tick as quickly as possible–not waiting for it to detach.
Symptoms Of Tickborne Illness
Many tickborne diseases can have similar signs and symptoms. If you get a tick bite and develop the symptoms below within a few weeks, see your healthcare provider.
The most common symptoms of tick-related illnesses include:
• Fever/chills. All tickborne diseases can cause fever.
• Aches and pains. Tickborne diseases can cause headache, fatigue, and muscle aches. People with Lyme disease may also have joint pain.
• Rash. Lyme disease, Southern tick-associated rash illness (STARI), Rocky Mountain spotted fever (RMSF), ehrlichiosis, and tularemia can cause distinctive rashes.
Your healthcare provider should evaluate the following before deciding on a plan for treatment:
• Your symptoms,
• the geographic region where you were bitten, and
• lab tests, depending on the symptoms and the geographic region where you were bitten.
Tick paralysis is thought to be caused by a toxin in the saliva of an attached tick. People with tick paralysis can experience weakness or paralysis that gradually moves up the body. These symptoms can sometimes resemble other neurologic conditions (for example, Guillain-Barré syndrome or botulism). Patients typically regain movement within 24 hours of removing the tick. .
Alpha-gal Syndrome
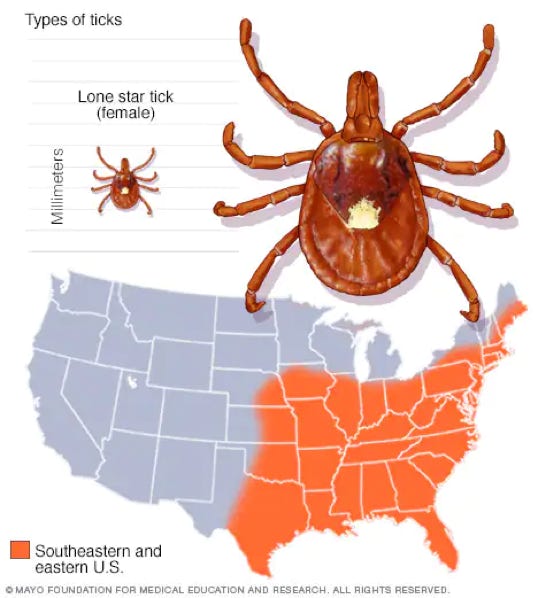
Note that alpha-gal is caused by the Lone Star Tick. This species is NOT currently in Arizona or New Mexico.
Products That May Contain Alpha-gal
What is alpha-gal?
• Alpha-gal (galactose-α-1,3-galactose) is a sugar molecule found in most mammals.
• Alpha-gal is not found in fish, reptiles, birds, or people.
• Alpha-gal can be found in meat (pork, beef, rabbit, lamb, venison, etc.) and products made from mammals (including gelatin, cow’s milk, and milk products).
What is alpha-gal syndrome (AGS)?
Alpha-gal syndrome (AGS) is a serious, potentially life-threatening allergic condition. AGS is also called alpha-gal allergy, red meat allergy, or tick bite meat allergy. AGS is not caused by an infection. AGS symptoms occur after people eat red meat or are exposed to other products containing alpha-gal.
A CDC report showed that between 2010 and 2022, more than 110,000 suspected cases of AGS were identified. However, cases of AGS are not nationally notifiable to CDC, so it is not known how many cases of AGS exist in the United States. Additional data and research are needed to understand how many people are affected by this condition.
What are the symptoms of AGS?
AGS reactions can include:
◦ Hives or itchy rash
◦ Nausea or vomiting
◦ Heartburn or indigestion
◦ Diarrhea
◦ Cough, shortness of breath, or difficulty breathing
◦ Drop in blood pressure
◦ Swelling of the lips, throat, tongue, or eye lids
◦ Dizziness or faintness
◦ Severe stomach pain
• Symptoms commonly appear 2-6 hours after eating meat or dairy products, or after exposure to products containing alpha-gal (for example, gelatin-coated medications).
• AGS reactions can be different from person-to-person. They can range from mild to severe or even life-threatening. Anaphylaxis (a potentially life-threatening reaction involving multiple organ systems) may need urgent medical care.
• People may not have an allergic reaction after every alpha-gal exposure.
• If you think you may have AGS go talk to your healthcare provider.
AGS can be severe, and even life-threatening. Seek immediate emergency care if you are having a severe allergic reaction.
Can I get AGS from a tick bite?
Alpha-gal syndrome is primarily associated with lone star tick (shown here), but other kinds of ticks have not been ruled out.
• Yes, AGS is associated with tick bites. Evidence suggests that AGS is primarily associated with the bite of a lone star tick in the United States, but other kinds of ticks have not been ruled out. Other tick species have been connected with the development of AGS in other countries.
• More research is needed to understand the role ticks play in starting this condition, and why certain people develop AGS.
How do I know if I have AGS?
• AGS is diagnosed by an allergist or other healthcare provider through a detailed patient history, physical examination, and a blood test that looks for specific antibodies (proteins made by your immune system) to alpha-gal.
• Your healthcare provider may also recommend allergy skin testing.
What should I do if I have AGS?
• AGS should be managed under the care of an allergist or other healthcare provider.
• Many foods and products contain alpha-gal. You will need to work with your healthcare provider to understand which products you need to avoid.
• Prevent tick bites. New tick bites may reactivate allergic reactions to alpha-gal.
I have AGS, what foods and products do I need to avoid?
• Not all patients with AGS have reactions to every ingredient containing alpha-gal.
• Most healthcare providers recommend patients with AGS stop eating mammalian meat (such as beef, pork, lamb, venison, rabbit, etc.).
• Depending on your sensitivity and the severity of your allergic reaction, your healthcare provider may also suggest you avoid other foods and ingredients which may contain alpha-gal (such as cow’s milk, milk-products, and gelatin).
• Read food product labels
carefully.
• Although very rare, some people with severe AGS may react to ingredients in certain vaccines or medications. Talk to your healthcare provider before taking a new medication or receiving a vaccine.
Who gets AGS?
Anyone can get AGS.
• Most reported cases of AGS in the United States are among people living in the South, East, and Central United States.
• While people in all age groups can develop AGS, most cases have been reported in adults.
What can I do to prevent AGS?
Preventing Tick Bites is important and may reduce your chances of developing AGS.
• Before you go outdoors
◦ Avoid grassy, brushy, and wooded areas, where ticks may be found.
◦ Walk in the center of trails.
◦ Treat clothing and gear with permethrin or buy pre-treated items.
◦ Use Environmental Protection Agency (EPA)-registered insect repellents
.
• After you come indoors
◦ Check your clothing for ticks.
◦ Examine gear and pets for ticks.
◦ Shower and perform a thorough tick check.
• If you see an attached tick, remove it immediately.
• Take steps to prevent ticks on your pets and in your yard.